Understanding Antibiotics: What They Are and How They Work
Antibiotics are a class of medications specifically designed to combat bacterial infections by inhibiting the growth of bacteria or killing them outright. They target essential biological functions unique to bacterial cells, such as cell wall synthesis, protein production, and DNA replication, while leaving human cells unharmed. This selective action is what makes antibiotics effective in treating various bacterial infections, ranging from mild ailments like strep throat to more severe conditions such as pneumonia.
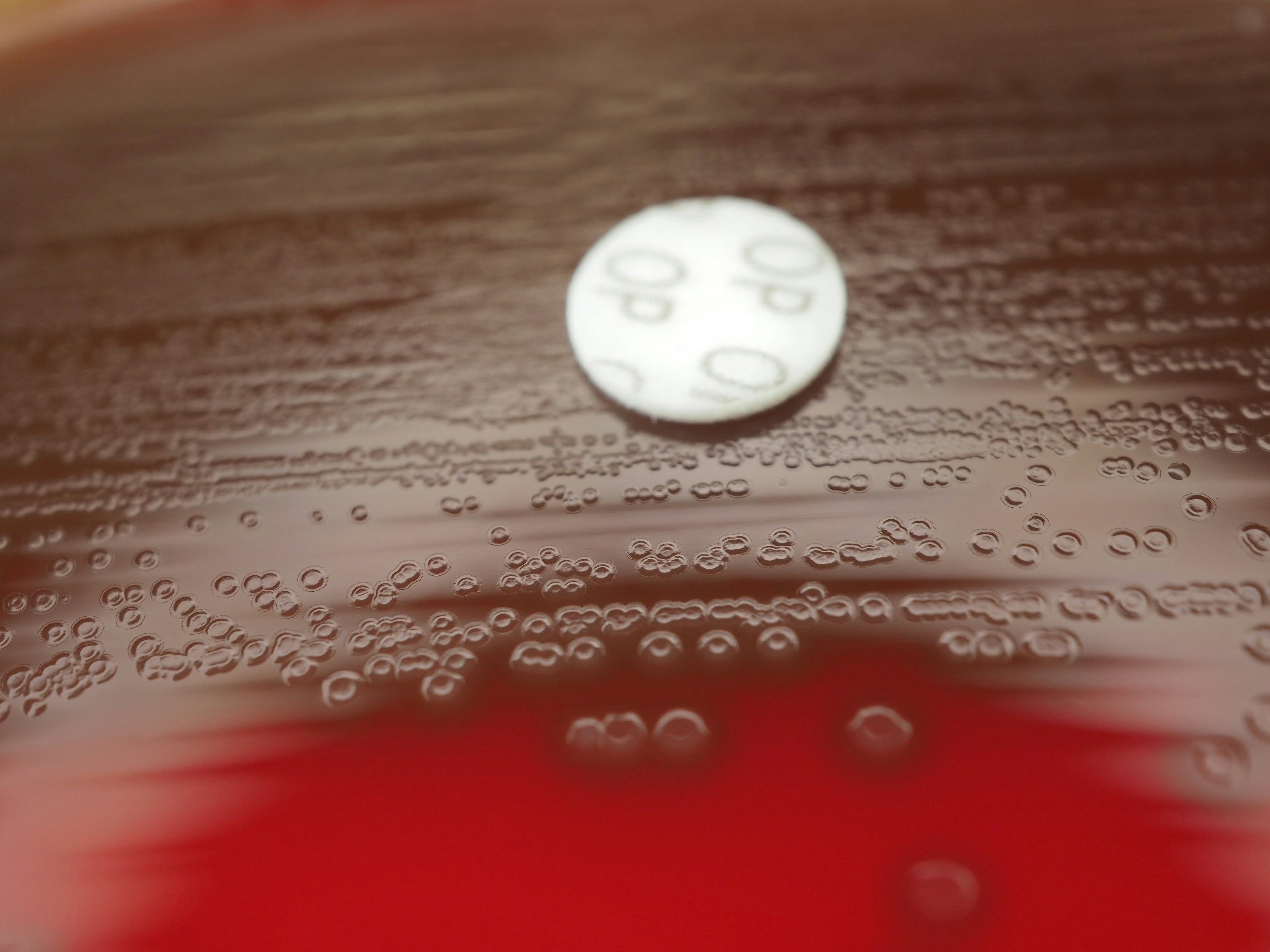
There are several types of antibiotics, broadly categorized into two main groups: bactericidal and bacteriostatic. Bactericidal antibiotics work by killing bacteria directly, which is crucial for serious infections where rapid bacterial elimination is needed. Common examples include penicillins and cephalosporins. On the other hand, bacteriostatic antibiotics inhibit bacterial growth and reproduction, allowing the body’s immune system to eliminate the pathogens more effectively. Tetracyclines and sulfonamides are well-known examples of this category. Understanding the difference between these types can help in choosing the appropriate treatment for specific infections.
A prevalent misconception about antibiotics is their effectiveness against viral infections, such as the common cold or influenza. Antibiotics have no effect on viruses and should not be used to treat viral sicknesses, as this can lead to unnecessary side effects and contribute to the growing concern of antibiotic resistance. Misuse and overuse of antibiotics can result in bacteria evolving and developing resistance to these medications, making future infections harder to treat. This makes it imperative to use antibiotics only when prescribed by a qualified healthcare professional, emphasizing the appropriate diagnosis of bacterial infections and ensuring their responsible use for effective treatment.
The Dangers of Antibiotic Overuse
Antibiotics serve a crucial role in the treatment of bacterial infections, but their overuse can lead to significant health risks and complications. One of the most alarming consequences of excessive antibiotic consumption is the development of antibiotic-resistant bacteria. When these drugs are used too frequently, especially for conditions that do not warrant their use, bacteria can adapt and evolve, becoming resistant to the effects of antibiotics. This resistance not only makes common infections more difficult to treat but also limits the effectiveness of existing antibiotics, posing a serious public health threat.
The phenomenon of antibiotic resistance contributes to a cycle where higher doses or alternative treatments are required, often leading to prolonged illnesses, increased healthcare costs, and greater risk of spreading resistant strains within communities. For instance, infections like urinary tract infections or certain strains of pneumonia may become harder to manage due to the diminishing effectiveness of standard antibiotic treatments. This trend raises urgent questions regarding our healthcare practices and necessitates more prudent antibiotic prescribing strategies.
In addition to the risk of resistance, the unnecessary use of antibiotics can lead to various side effects. Common short-term side effects include gastrointestinal disturbances, such as nausea or diarrhea, which can impact the quality of life for patients. More long-term complications can also arise, such as disruption to the normal microbiota of the gut, which can lead to further health complications, including infections caused by opportunistic pathogens like Clostridium difficile. The potential for serious side effects underlines the need for caution when prescribing and using these powerful medications.
Ultimately, the dangers surrounding the overuse of antibiotics extend beyond individual health concerns, highlighting a broader issue within our medical systems. Responsible use of antibiotics is essential to ensure their continued effectiveness and to safeguard public health.
Responsible Antibiotic Use: Guidelines and Recommendations
Antibiotics remain a crucial component of modern medicine, providing effective treatment for a variety of bacterial infections. However, responsible use is imperative to mitigate the risk of antibiotic resistance and minimize the potential side effects associated with these medications. To ensure antibiotics are used judiciously, several guidelines and recommendations can be followed by both patients and healthcare providers.
Firstly, it is essential for individuals to recognize when antibiotics are truly necessary. Antibiotics are effective against bacterial infections but will not alleviate symptoms associated with viral infections such as colds or influenza. Patients should consult with healthcare providers to make informed decisions about whether antibiotics are warranted for their specific symptoms or conditions. This collaborative approach encourages appropriate use and can help prevent unnecessary prescriptions.
Furthermore, if an antibiotic is prescribed, it is crucial to follow the treatment plan meticulously. This means taking the medication exactly as directed, which includes adhering to the prescribed dose, frequency, and duration. Completing the entire course of antibiotics is vital—even if symptoms improve before finishing the medication. Incomplete treatment can promote the development of antibiotic resistance, as surviving bacteria may adapt and become harder to eradicate in future infections.
Additionally, patients are encouraged to engage in open discussions with their healthcare providers regarding any concerns about side effects or potential interactions with other medications. Awareness and communication can foster a supportive environment where patients feel comfortable asking questions and expressing their apprehensions.
Lastly, advocating for responsible antibiotic use extends beyond individual actions. Patients can contribute to public health efforts by practicing preventive measures, such as vaccination and maintaining proper hygiene, thereby reducing the need for antibiotics overall. In conclusion, being informed and proactive about antibiotic use is essential in combating resistance and ensuring effective treatment for future generations.
The Future of Antibiotics and Alternatives
The field of antibiotics is undergoing significant evolution, prompted by the urgent need to address antibiotic resistance and the limitations of traditional antibiotics. Various research initiatives are exploring innovative therapeutic approaches that extend beyond conventional drugs. One promising area is phage therapy, which utilizes bacteriophages—viruses that target and destroy specific bacteria. This method has the potential to treat antibiotic-resistant infections effectively, providing a targeted treatment option that minimizes collateral damage to the body’s microbiome.
Additionally, advancements in vaccine development are proving essential in preventing bacterial infections that often necessitate antibiotic treatment. By vaccinating against specific pathogens, we can reduce the incidence of infections, thereby lowering the overall demand for antibiotics. This strategy, combined with ongoing research into new non-antibiotic treatments, aims to revolutionize our approach to infection management and antibiotic usage.
Education plays a vital role in combating antibiotic resistance and ensuring the responsible use of existing antibiotics. Healthcare providers must be well-informed about the implications of antibiotic overuse and the potential side effects associated with various treatments. Public awareness campaigns can also help patients understand the importance of adhering to prescribed treatment regimens while avoiding unnecessary antibiotic consumption.
Moreover, research into alternative therapies continues to gain traction. For instance, compounds derived from natural sources—such as plants or fungi—are being studied for their potential to offer similar benefits without contributing to resistance. These alternatives could serve as adjunct therapies or even replace traditional antibiotics in certain cases.
In conclusion, the future of antibiotics relies on embracing innovative approaches and prioritizing education. By investing in research and promoting alternative treatments, we can uphold the efficacy of antibiotics and ensure their effectiveness for future generations, while mitigating the risks associated with resistance and side effects.